Portal User Manual – Eligibility Check
Need help?
Contact Us About Claims
Claim Status/Patient Eligibility:
(866) 518-3285
24 hours a day, 7 days a week
Claim Corrections:
(866) 518-3253
7:00 am to 4:30 pm CT M-Th
DDE Navigation & Password Reset: (866) 518-3251
7:00 am to 4:30 pm CT M-F
DDE System Access: (866) 518-3295
7:00 am to 4:30 pm CT M-F
EDI: (866) 518-3285
7:00 am to 5:00 pm CT M-F
General Inquiries:
(866) 518-3285
7:00 am to 5:00 pm CT M-F
Claim Status/Patient Eligibility:
(866) 234-7331
24 hours a day, 7 days a week
Claim Corrections:
(866) 580-5980
8:00 am to 5:30 pm ET M-Th
DDE Navigation & Password Reset: (866) 580-5986
8:00 am to 5:30 pm ET M-F
DDE System Access: (866) 518-3295
8:00 am to 5:30 pm ET M-F
EDI: (866) 234-7331
8:00 am to 5:00 pm ET M-F
General Inquiries:
(866) 234-7331
8:00 am to 5:00 pm ET M-F
Claim Status/Patient Eligibility:
(866) 518-3285
24 hours a day, 7 days a week
Claim Corrections/Reopenings:
(866) 518-3285
7:00 am to 5:00 pm CT M-F
EDI: (866) 518-3285
7:00am to 5:00 pm CT M-F
General Inquiries:
(866) 518-3285
7:00 am to 5:00 pm CT M-F
Claim Status/Patient Eligibility:
(866) 234-7331
24 hours a day, 7 days a week
Claim Corrections/Reopenings:
(866) 234-7331
8:00 am to 5:00 pm ET M-F
EDI: (866) 234-7331
8:00 am to 5:00 pm ET M-F
General Inquiries:
(866) 234-7331
8:00 am to 5:00 pm ET M-F
Need help?
General questions about Medical Review
 (866) 518-3285
(866) 518-3285
7:00 am to 5:00 pm CT M-F
 (866) 234-7331
(866) 234-7331
8:00 am to 5:00 pm ET M-F
 (866) 518-3285
(866) 518-3285
7:00 am to 5:00 pm CT M-F
 (866) 234-7331
(866) 234-7331
8:00 am to 5:00 pm ET M-F
Need help?
Contact Us About Overpayments
Inquiries regarding refunds to Medicare - MSP Related
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Secondary.Payer.Inquiry@wpsic.com
Inquiries regarding overpayments NOT associated with MSP
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Reimbursement.Overpayment.
Inquiry@wpsic.com
Inquiries regarding refunds to Medicare - MSP Related
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Secondary.Payer.Inquiry@wpsic.com
Inquiries regarding overpayments NOT associated with MSP
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Reimbursement.Overpayment.
Inquiry@wpsic.com
Questions regarding overpayments associated with MSP related debt
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Secondary.Payer.Inquiry@wpsic.com
Questions regarding overpayments NOT associated with MSP related debt
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 6:00pm ET) M-Fri
Payment.Recovery.Inquiry@wpsic.com
Questions regarding overpayments associated with MSP related debt
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-Fri
Secondary.Payer.Inquiry@wpsic.com
Questions regarding overpayments NOT associated with MSP related debt
(866) 234-7331
8:00 am to 5:00 pm ET (7:00 am to 4:00pm CT) M-Fri
Payment.Recovery.Inquiry@wpsic.com
Need help?
Contact us about Appeals
7:00 am to 5:00 pm CT M-F
8:00 am to 5:00 pm ET M-F
7:00 am to 5:00 pm CT M-F
8:00 am to 5:00 pm ET M-F
Need help?
Contact Us About Provider Enrollment
(866) 518-3285
7:00 AM - 5:00 PM CT, Monday - Friday
USPS Mailing Address
WPS GHA
Medicare Provider Enrollment
P.O. Box 8248
Madison, WI 53708-8248
Overnight Delivery
WPS GHA
Medicare Provider Enrollment
1717 W. Broadway
Madison, WI 53713-1834
(866) 234-7331
8:00 AM - 5:00 PM ET, Monday - Friday
USPS Mailing Address
WPS GHA
Medicare Provider Enrollment
P.O. Box 8248
Madison, WI 53708-8248
Overnight Delivery
WPS GHA
Medicare Provider Enrollment
1717 W. Broadway
Madison, WI 53713-1834
(866) 518-3285
7:00 AM - 5:00 PM CT, Monday - Friday
USPS Mailing Address
WPS GHA
Medicare Provider Enrollment
P.O. Box 8248
Madison, WI 53708-8248
Overnight Delivery
WPS GHA
Medicare Provider Enrollment
1717 W. Broadway
Madison, WI 53713-1834
(866) 234-7331
8:00 AM - 5:00 PM ET, Monday - Friday
USPS Mailing Address
WPS GHA
Medicare Provider Enrollment
P.O. Box 8248
Madison, WI 53708-8248
Overnight Delivery
WPS GHA
Medicare Provider Enrollment
1717 W. Broadway
Madison, WI 53713-1834
Need help?
Contact us about Policies
 (866) 518-3285 - General questions about Policies
(866) 518-3285 - General questions about Policies
7:00 am to 5:00 pm CT M-F
 (866) 234-7331 - General questions about Policies
(866) 234-7331 - General questions about Policies
8:00 am to 5:00 pm ET M-F
 (866) 518-3285 - General questions about Policies
(866) 518-3285 - General questions about Policies
7:00 am to 5:00 pm CT M-F
 (866) 234-7331 - General questions about Policies
(866) 234-7331 - General questions about Policies
8:00 am to 5:00 pm ET M-F
LCD Reconsideration Request: Policycomments@wpsic.com
Draft LCD Comments: Policycomments@wpsic.com
IDE Submissions: IDE.mailbox@wpsic.com
RSVP for Open Meeting and CAC: LCDCAC@wpsic.com
Questions about Payments and Incentive Programs
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Contact us about Form CMS-588 Electronic Funds Transfer (EFT)
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Financial.Reporting.Inquiry@wpsic.com
Do not submit PHI/PII through email
Questions about Payments and Incentive Programs
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Contact us about Form CMS-588 Electronic Funds Transfer (EFT)
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Financial.Reporting.Inquiry@wpsic.com
Do not submit PHI/PII through email
Questions about Payments, Fee Schedules, and Incentive Programs
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Contact us about Form CMS-588 Electronic Funds Transfer (EFT)
(866) 518-3285
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Financial.Reporting.Inquiry@wpsic.com
Do not submit PHI/PII through email
Questions about Payments, Fee Schedules, and Incentive Programs
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Contact us about Form CMS-588 Electronic Funds Transfer (EFT)
(866) 234-7331
7:00 am to 5:00 pm CT (8:00 am to 5:00 pm ET) M-F
Financial.Reporting.Inquiry@wpsic.com
Do not submit PHI/PII through email
Need help?
Need help?
Mail audit materials:
WPS GHA
ATTN: Audit Supervisor
P.O. Box 8696
Madison, WI 53708-8696
When using a delivery service:
WPS GHA
ATTN: Audit Supervisor
1717 W. Broadway
Madison, WI 53713-1834
Mail audit materials:
WPS GHA
ATTN: Audit Supervisor
P.O. Box 14172
Madison, WI 53708-0172
When using a delivery service:
WPS GHA
ATTN: Audit Supervisor
1717 W. Broadway
Madison, WI 53713-1834
Need help?
Try these links first.
Questions about Self-Service?
(866) 518-3285
7:00 am to 5:00 pm CT M-F
Try these links first.
Questions about Self-Service?
(866) 518-3285
7:00 am to 5:00 pm CT M-F
Try these links first.
Questions about Self-Service?
(866) 234-7331
8:00 am to 5:00 pm ET M-F
Try these links first.
Questions about Self-Service?
(866) 234-7331
8:00 am to 5:00 pm ET M-F
Portal User Manual – Eligibility Check
You currently have jurisdiction selected, however this page only applies to these jurisdiction(s): .
Print the complete Portal User Manual ![]()
Eligibility Check allows providers to verify certain information Medicare has on file for Medicare beneficiaries. This information helps providers bill Medicare correctly. Information is generally available 24 hours a day but may be temporarily unavailable due to scheduled or unscheduled maintenance.
Sources of Eligibility Data
The eligibility information available in the WPS Government Health Administrators Portal comes from the HIPAA Eligibility Transaction System (HETS) 270/271 eligibility transaction. The information available in the portal is the same information provided by the Interactive Voice Response (IVR). It is important to understand that while eligibility information is accurate at the time it is given, the information may change if Medicare (or any of the Federal agencies that supply data to HETS, such as the Social Security Administration) receives additional information. Although the data from HETS is updated in real time, the data comes from many different sources that may take up to two weeks to update. Medicare contractors process claims based on the information on Medicare’s files at the time the claim is processed.
If you have a question about a patient’s eligibility information, you or the patient should contact the entity responsible for providing the data to Medicare:
- Contact the Social Security Administration for questions about Medicare entitlement or benefit dates.
- Contact the Benefits Coordination and Recovery Center (BCRC) for Medicare Secondary Payer (MSP) questions. The BCRC can also assist with some issues involving Medigap or supplemental insurance (i.e., insurance that pays after Medicare).
- Contact the Medicare Advantage (MA) plan (i.e., Managed Care Organization or Medicare replacement plan) directly for all questions involving MA plans.
- Contact your state’s Medicaid agency for questions about the Qualified Medicare Beneficiary (QMB) program.
Accessing Eligibility Check
You can access Eligibility Check by clicking on the link under the My Transactions heading in the left navigation menu.

After clicking the link, select your service location (if it is not already prepopulated) and enter the following information about your patient:
- Medicare number (i.e., the Medicare Beneficiary Identifier (MBI))
- First name -OR- Date of birth
- Last name
- Suffix, if applicable (e.g., Jr., Sr., III, etc.)
- Starting and ending dates of service (DOS)
NOTE: The eligibility information provided corresponds to the starting and ending dates of service you enter on the search screen. You can search for eligibility information up to four years in the past or 4 months in the future by changing the dates in the Starting DOS and Ending DOS fields.
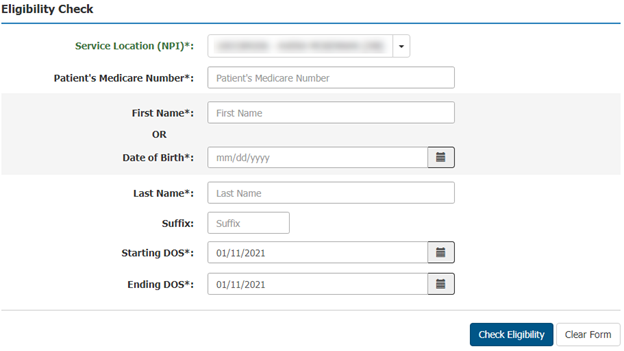
Click the Check Eligibility button to start the search. If any of the information you entered is incorrect, you will see an error message.
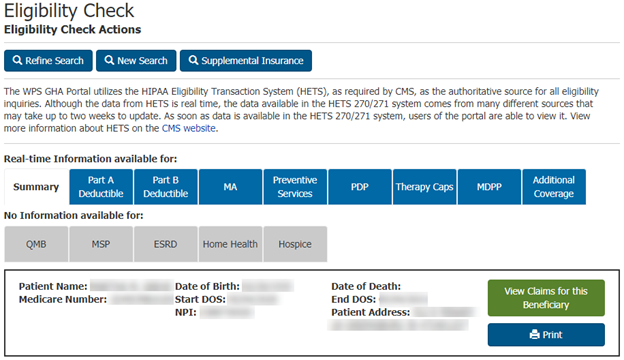
If the information you entered is valid, the portal will display the beneficiary’s basic details along with links to additional eligibility categories.
- The category box is blue if eligibility information is available.
- The category box is gray if no eligibility information is available in that category.
You can also refine your search or start a new one, jump to the Claim Inquiry page (which will be prepopulated with the beneficiary’s Medicare number), or print the beneficiary’s eligibility details from this screen.
Available Eligibility Information
Use the tabs located above the patient’s details to see additional eligibility information for your patient. The tabs highlighted in blue contain additional information for your patient. The order of the tabs will vary depending on the eligibility information available. The information available includes:
- Eligibility summary
- Part A deductible
- Part B deductible
- Medicare Advantage (MA) plan enrollment
- Preventive services eligibility
- Prescription drug plan (PDP) information
- Therapy cap (threshold) information
- Medicare Diabetes Prevention Program (MDPP) eligibility
- Acupuncture eligibility (on the Additional Coverage tab)
- Cognitive Assessment and Care Plan Services (on the Additional Coverage tab)
- Qualified Medicare Beneficiary (QMB) program eligibility
- Medicare Secondary Payer (MSP) information
- End stage renal disease (ESRD) eligibility
- Home health eligibility
- Hospice eligibility
- Part B Immunosuppressant Drug (PBID)
- Supplemental insurance information
NOTE: Medicare Diabetes Prevention Program (MDPP) suppliers have limited access to eligibility information. The data available is limited to the information an MDPP supplier would need to bill for MDPP services: Part B eligibility date, managed care organization (MCO) data, Medicare secondary payer (MSP) data, and end-stage renal disease (ESRD) data.
Summary

The Summary tab provides the following entitlement and benefit information:
- Part A and Part B entitlement dates
- Part A and Part B entitlement reason codes (Hover your mouse over the code to display the definition of the reason code.)
- Previous Part A and Part B entitlement dates
- Part A and Part B ineligible dates (A beneficiary may have periods of ineligibility during their Medicare entitlement. The portal will show periods of ineligibility occurring within your search parameters.)
- Part A benefit data:
- Lifetime reserve days
- Lifetime reserve co-payment amount
- Lifetime psychiatric days
- Hospital days
- Hospital co-payment days and amount
- Skilled nursing facility (SNF) days
- Skilled nursing facility (SNF) co-payment days and amount
- Part B benefit data:
- Pulmonary rehabilitation sessions
- Blood deductible
- Smoking cessation sessions
- Cardiac rehabilitation sessions
- Intensive cardiac rehabilitation sessions
- Link to a list of procedure codes that require Prior Authorization
Return to Available Eligibility Information
Part A Deductible

The Part A Deductible tab provides the following information:
- Coverage time span (year)
- Part A deductible amount
- Hospital spell dates (earliest/latest billing date and days remaining) and deductible remaining
- Hospital co-payment amount and days remaining
- Hospital stay dates and billing NPI
- SNF spell dates (earliest/latest billing date and days remaining) and deductible remaining
- SNF co-payment amount and days remaining
- SNF stay dates and billing NPI
Return to Available Eligibility Information
Part B Deductible
The Part B Deductible tab provides the following information:
- Coverage time span (year)
- Part B deductible amount
- Part B deductible remaining
Return to Available Eligibility Information
Medicare Advantage (MA)

The MA tab provides information about insurance that pays INSTEAD of Medicare. This type of insurance is known by many names, including Medicare Part C, Medicare HMO, Medicare managed care organization, Medicare health plan, or Medicare replacement plan. When a beneficiary enrolls in a Medicare Advantage plan, they remain enrolled in Medicare, but they elect to have their Medicare-covered services processed and paid by another insurer. In exchange for allowing the other insurer to manage their care (which usually includes limiting the beneficiary to a network of providers), the beneficiary may receive additional benefits that aren’t covered under Original Medicare. In most cases, the provider submits a claim only to the MA plan. Though uncommon, some MA plan options allow beneficiaries to see out-of-network providers and have those services processed by Original Medicare instead of by the MA plan.
The MA tab provides the following information:
- MA plan enrollment and termination dates
- MA contract and plan
- MA name, address, telephone number, and website (if available)
- MA enrollment plan type
- Bill option code
- MA and plan benefit package (PBP) information are displayed on separate lines
Return to Available Eligibility Information
Preventive Services

The Preventive Services tab provides the following information about the preventive services Medicare covers subject to specific frequency limitations (e.g., repeat preventive services covered only after a set amount of time has passed):
- Procedure code (with professional/technical modifier, if applicable)
- Next eligible date
- Pneumococcal pneumonia vaccination history (procedure code, rendering provider’s NPI, and date of service)
- Influenza (procedure code, rendering provider’s NPI, and date of service)
- COVID-19 Immunization Data (procedure code, immunization date, and rendering provider’s NPI)
The portal displays current eligibility data only. You should not infer historic eligibility or prior services rendered based on the next eligible date. (For example, do not infer that the patient previously received a colonoscopy based on the date the patient is next eligible for a colonoscopy.)
If a procedure code has different next eligible dates for the professional and technical components, the portal will display different eligibility dates for each component.
The portal displays the procedure codes that may be used to bill for preventive services that have a specific frequency limitation, including:
- Alcohol misuse screening and counseling (G0442 and G0443)
- Annual Wellness Visit (AWV) (G0438 and G0439)
- Audiology Screening (92550, 92552, 92553, 92555, 92556, 92557, 92562, 92563, 92565, 92567,92568, 92570, 92571, 92572, 92575, 92576, 92577, 92579, 92582, 92583, 92584, 92587, 92588, 92601, 92602, 92603, 92604, 92620, 92621, 92625, 92626, 92627, 92640, 92651, 92652, and 92653)
- Bone mass measurement (76977, 77078, 77080, 77081, and G0130)
- Cardiovascular disease screening (80061, 82465, 83718, and 84478)
- Colorectal cancer screening (G0104, G0105, G0106, G0120, G0121, G0327, G0328, and 82270)
- Depression screening (G0444)
- Diabetes screening (82947, 82950, and 82951)
- Glaucoma screening (G0117 and G0118)
- Hepatitis B screening (G0499)
- Hepatitis C screening (G0472)
- Human Immunodeficiency Virus (HIV) screening (G0475)
- Intensive behavioral therapy (IBT) for cardiovascular disease (CVD) (G0446)
- Intensive behavioral therapy for obesity (G0447)
- Initial Preventive Physical Examination (IPPE) (G0402, G0403, G0404, and G0405)
- Prostate cancer screening (G0102 and G0103) (males only)
- Screening for cervical cancer with human papillomavirus (HPV) (G0476) (females only)
- Screening for sexually transmitted infections (STIs) and high intensity behavioral counseling (HIBC) to prevent STIs (G0445)
- Screening mammography (77067)
- Screening Pap tests (G0123, G0143, G0144, G0145, G0147, G0148, P3000, and Q0091)
- Screening pelvic exam (G0101)
- Ultrasound screening for abdominal aortic aneurysm (AAA) (76706)
For more information about preventive services, including those services that are not included on the Preventive Services tab, see the Medicare Preventive Services tool on the CMS website.
Return to Available Eligibility Information
Prescription Drug Plan (PDP)

The PDP tab provides information about any Medicare Part D prescription drug plans the beneficiary has enrolled in. While these plans are called Medicare Part D, they are stand-alone prescription drug plans offered by private insurers, not Original Medicare. Providers who have questions about a patient’s PDP should contact the PDP insurer directly. The PDP tab provides the following information:
- PDP enrollment and termination dates
- PDP contract and plan numbers
- Part D insurer’s contact information, including:
- Insurer’s name
- Insurer’s address
- Insurer’s telephone number
- Insurer’s website (if available)
- PDP plan name
Return to Available Eligibility Information
Therapy Caps

The Therapy Caps tab provides information about the annual per-beneficiary threshold limitations on physical therapy (PT), occupational therapy (OT), and speech-language pathology (SLP) services. In previous years, Medicare set financial limitations on the therapy services beneficiaries could receive in a calendar year. The Bipartisan Budget Act (BBA) of 2018 repealed those caps and added a limitation to ensure beneficiaries receive appropriate therapy. Though it is more accurate to refer to the limitations as per-beneficiary thresholds or KX modifier thresholds, they are commonly called “therapy caps.”
There are two separate thresholds for therapy services: One for PT and SLP services combined and another for OT services. The Therapy Caps tab provides the following information:
- Type of therapy (Note: While the types of therapy are labeled either occupational therapy or physical therapy on this screen, remember physical therapy also includes speech-language pathology services)
- Deductible year
- Amount applied toward threshold (labeled “Part B Therapy Cap Used”)
Return to Available Eligibility Information
Medicare Diabetes Prevention Program (MDPP)

The MDPP tab provides information about Medicare Diabetes Prevention Program (MDPP) eligibility. The MDPP is a once in a lifetime benefit for eligible beneficiaries at risk of developing type 2 diabetes. Medicare Part B covers an initial 12-month period (six months of weekly sessions followed by six additional months of monthly sessions). Medicare can also cover a second 12-month period of maintenance sessions if the beneficiary meets certain criteria.
The MDPP tab provides the following information:
- MDPP effective and termination dates
- Inactive coverage
- Active coverage
- MDPP HCPCS codes billed
- Billing Provider NPI
- Date of Service for each HCPCS code
- MDPP Period 2 End Date
NOTE: The effective date for active coverage only displays the starting date of service you submitted on your eligibility request. It is NOT the actual start date for the beneficiary’s MDPP. If the beneficiary’s MDPP enrollment is not active, it will display the starting date of service submitted on your eligibility request on the Inactive Coverage line.
Return to Available Eligibility Information
Additional Coverage

The Additional Coverage tab provides information about Medicare’s coverage of acupuncture for chronic low back pain. Medicare Part B covers up to 12 acupuncture visits in 90 days to treat low back pain. Medicare can also cover 8 additional sessions if the initial sessions improve the beneficiary’s low back pain. No more than 20 acupuncture treatments are covered annually.
Also found on the Additional Coverage tab is Cognitive Assessment and Care Plan services data provided there is not a recorded date of death prior to or equal to the requested date(s) of service. If there are no services provided during the request date(s) of service but there is prior usage, the portal will include the most recent service occurrence.
The Additional Coverage tag provides the following information:
Acupuncture:
- Technical sessions remaining
- Next technical date
- Professional sessions remaining
- Next professional date
Cognitive Assessment and Care Plan:
- HCPCS 99483
- Date of service
- Rendering provider NPI
Return to Available Eligibility Information
Qualified Medicare Beneficiary (QMB)

The QMB tab provides information Qualified Medicare Beneficiary (QMB) eligibility. A QMB is eligible for both Medicare and Medicaid. Medicare providers and suppliers may not bill people in the QMB program for Medicare deductibles, coinsurance, or copays. Providers may be eligible to bill state Medicaid programs for those costs. People in the QMB program have no legal obligation to pay Medicare providers for Medicare Part A or Part B cost-sharing amounts even if the provider is not enrolled in the state’s Medicaid program. For more information, see the CMS website.
The QMB tab provides the following information:
- QMB enrollment period
NOTE: State Medicaid agencies determine QMB eligibility monthly, but they may not update the systems that supply eligibility data to Medicare by the first day of each month.
Return to Available Eligibility Information
Medicare Secondary Payer (MSP)

The MSP tab provides information about insurance that pays BEFORE Medicare pays. When a beneficiary has two or more insurers, there are rules that determine which insurer pays first. Some types of primary insurance, such as employer group health plans, pay before Medicare for all types of services. Other types of primary insurance, such as worker’s compensation or liability insurance, only pay before Medicare for services related to an accident or injury. In most cases, the provider submits a claim to the MSP insurer first and then submits a claim to Medicare. For more information, see the CMS website. ![]()
See our Medicare Secondary Payer (MSP) Fact Sheet for information on determining who is Primary to Medicare.
The MSP tab provides the following information:
- Enrollment and termination dates
- Insurer name and address
- Insurance type code and description
- Policy ID
- Group Number
- Last MSP Maintenance Date
- Patient Relationship Code
- MSP Source Code
- Diagnosis codes associated with the beneficiary’s accident or injury
- ORM Indicator
Return to Available Eligibility Information
End Stage Renal Disease (ESRD)

The ESRD tab provides eligibility information for beneficiaries eligible for Medicare due to their end stage renal disease. Medicare eligibility due to ESRD works differently than other types of Medicare eligibility. Medicare’s coverage depends on when the beneficiary begins or ends regular dialysis treatments or receives a kidney transplant. For more information about Medicare eligibility due to ESRD, see the CMS website.
The ESRD tab provides the following information:
- ESRD coverage period effective date and end date
- Dialysis start and end date (if applicable)
- Kidney transplant date (if applicable)
Return to Available Eligibility Information
Home Health

The Home Health tab provides information about home health periods of care. Home health agencies (HHAs) submit a consolidated bill to Medicare for the home health services a beneficiary receives during a home health episode of care. With limited exceptions, Medicare will only pay the HHA for the home health services and medical supplies a beneficiary receives during each 30-day period of care. For more information, see the CMS website. ![]()
The Home Health tab provides the following information:
- Home health period start and end dates
- Date of earliest and latest billing activity
- HHA provider NPI
- Contractor number and name
- Patient status code (indicating whether the beneficiary is actively receiving services)
- Notice of Admissions (NOA) Indicator
- 1 – NOA Received without condition code 47
- 2 – NOA received with condition code 47
Return to Available Eligibility Information
Hospice

The Hospice tab provides information about benefit periods once a beneficiary elects to receive hospice care. When a beneficiary elects to receive hospice care, they agree to receive palliative care instead of treatment to cure their terminal illness. Hospice care is available for two periods of 90 days and an unlimited number of subsequent 60-day periods. For more information, see the CMS website.
The Hospice tab provides the following information:
Hospice Election Period Information (The Hospice Election Revocation Indicator will now be sourced from the specific Hospice Election record instead of the Hospice Period record):
- Hospice provider NPI
- Start date
- Receipt date
- Revocation date
- Revocation code
Hospice Benefit Period Information:
- Benefit period provider NPI
- Start and end date
- Dates of earliest and latest billing activity
- Number of hospice days used
Return to Available Eligibility Information
Part B Immunosuppressant Drug (PBID)

The PBID tab provides Enrollment information for Medicare beneficiaries following a kidney transplant. This benefit provides coverage for immunosuppressant drugs beyond the 36 months following a kidney transplant. This will only cover immunosuppressive drugs and no other services or items. The HETS response will return up to ten (10) Part B-ID enrollment periods within the requested date(s) of service. The HETS response for Part B-ID will never include Medicare Advantage (MA) or Medicare Secondary Payer (MSP) data.
The PBID tab provides the following information:
- Enrollment Reason Code
- Coverage Time Span
- Deductible Base
- Deductible Remaining
- Coinsurance
Return to Available Eligibility Information
Supplemental Insurance
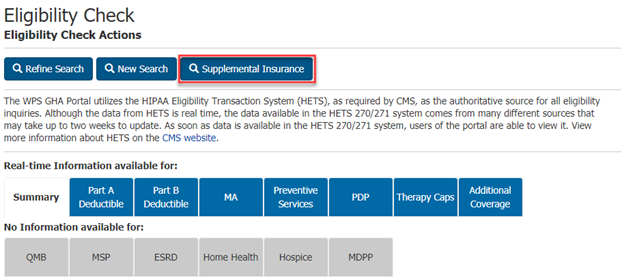
The Supplemental Insurance button provides information about insurance that may pay for services after Medicare processes the claim. Unlike the other eligibility information, the supplemental insurance information is available by clicking a button located above the row of eligibility information tabs.
The supplemental insurance information available is for informational purposes only. It may not be a comprehensive list of any or all the supplemental insurance a beneficiary may have. Medicare’s information is limited to Medicare Crossover trading partners that sign trading partner agreements with Medicare. A trading partner agreement allows Medicare to send claim information to the supplemental insurer after Medicare processes the claim. Beneficiaries may have other insurance that would require the provider to file a claim directly with the insurer. Providers should obtain supplemental insurance information from the beneficiary.
The Supplemental Insurance tab provides the following information:
- Supplemental insurer’s name and address
- Supplemental insurance effective and termination date
- Coordination of benefits agreement (COBA) number
global-tags: J8A,J5A,J8B,J5B
.
View AMA License
LICENSE FOR USE OF PHYSICIANS' CURRENT PROCEDURAL TERMINOLOGY, FOURTH EDITION (CPT)
End User Point and Click Agreement:
CPT codes, descriptions and other data only are copyright 2022 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association (AMA).
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of Centers for Medicare and Medicaid Services (CMS) internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by CMS. You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, 515 N. State Street, Chicago, IL 60654. Applications are available at the AMA Web site, http://www.ama-assn.org/go/cpt.
Applicable FARS\DFARS Restrictions Apply to Government Use. This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60654. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2) (November 1995) and/or subject to the restrictions of DFARS 227.7202-1(a) (June 1995) and DFARS 227.7202-3(a) (June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT should be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking above on the button labeled "Accept".
LICENSE FOR USE OF CURRENT DENTAL TERMINOLOGY (CDT™)
These materials contain Current Dental Terminology (CDTTM), Copyright © 2010 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING ABOVE ON THE BUTTON LABELED "ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees and agents are authorized to use CDT only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CDT for resale and/or license, transferring copies of CDT to any party not bound by this agreement, creating any modified or derivative work of CDT, or making any commercial use of CDT. License to use CDT for any use not authorized herein must be obtained through the American Dental Association, 211 East Chicago Avenue, Chicago, IL 60611. Applications are available at the American Dental Association web site, http://www.ADA.org/.
- Applicable Federal Acquisition Regulation Clauses (FARS)\Department of restrictions apply to Government Use. Please click here to see all U.S. Government Rights Provisions.
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT IS PROVIDED "AS IS" WITHOUT WARRANTY OF ANY KIND, EITHER EXPRESSED OR IMPLIED, INCLUDING BUT NOT LIMITED TO, THE IMPLIED WARRANTIES O F MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE. NO FEE SCHEDULES, BASIC UNIT, RELATIVE VALUES OR RELATED LISTINGS ARE INCLUDED IN CDT. THE ADA DOES NOT DIRECTLY OR INDIRECTLY PRACTICE MEDICINE OR DISPENSE DENTAL SERVICES. THE SOLE RESPONSIBILITY FOR THE SOFTWARE, INCLUDING ANY CDT AND OTHER CONTENT CONTAINED THEREIN, IS WITH (INSERT NAME OF APPLICABLE ENTITY) OR THE CMS; AND NO ENDORSEMENT BY THE ADA IS INTENDED OR IMPLIED. THE ADA EXPRESSLY DISCLAIMS RESPONSIBILITY FOR ANY CONSEQUENCES OR LIABILITY ATTRIBUTABLE TO OR RELATED TO ANY USE, NON-USE, OR INTERPRETATION OF INFORMATION CONTAINED OR NOT CONTAINED IN THIS FILE/PRODUCT. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT should be addressed to the ADA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. IN NO EVENT SHALL CMS BE LIABLE FOR DIRECT, INDIRECT, SPECIAL, INCIDENTAL, OR CONSEQUENTIAL DAMAGES ARISING OUT OF THE USE OF SUCH INFORMATION OR MATERIAL.